- Conflict:
- Vietnam War (1962-73)
- Services:
- Army, Air Force, Navy, Nursing services
In 1953, Captain Dita McCarthy, an Australian Army nurse, was posted to the British Commonwealth hospital near Seoul. The hospital, not far from the Korean War front line, received a constant stream of wounded soldiers. Many arrived on stretchers tied onto the back of Jeeps, having endured a long ride on Korea’s primitive and congested roads. A few were able to be evacuated by helicopter. The helicopters available did not have room in the cabin for a stretcher so patients were placed in pods slung beneath the aircraft. Medical attention during the flight was impossible.
The hospital, a former school, had primitive working and living conditions. There was no running water, and, at first, no heating. The electrical generator rarely worked and the nurses’ night rounds were carried out with a hurricane lamp—a scene reminiscent of Florence Nightingale in the Crimean War. There was no ability to sterilise medical instruments and no equipment for general anaesthesia. McCarthy recalled:
We all wanted to do more for ‘our boys’ but were restricted by a lack of facilities or resources. As the war progressed... the wounded were becoming younger and younger.
To make matters worse, the nurses, the first women to arrive in what had been an all-male hospital, encountered prejudice and chauvinism from some of their male colleagues. It took some heated confrontations before the women gradually became accepted as part of the team.
The doctors and nurses in Seoul did what they could with the equipment available. For any major surgery, patients had to be sent to the British Commonwealth hospital at Kure in Japan—a long flight in a Dakota aircraft.
On 2 September 2008, the Australians in Afghanistan suffered their largest number of casualties in a single day. Nine Australians were wounded at the battle of Ana Kalay, when an SAS patrol came under sustained enemy attack. As soldiers were given immediate first aid, requests for medical evacuation were made. These came through to the Role 2a medical facility at Tarin Kowt, the main Australian base in Afghanistan, an austere but well equipped facility. The Commanding Officer immediately activated the Mass Casualty Plan and called all available personnel to duty.
The wounded soldiers arrived in Black Hawk helicopters dedicated to medical evacuation. As they arrived, then Wing Commander Annette Holian, as Clinical Director, performed triage. She assessed the condition of every soldier as he came in, marking their medical priority in marker pen on their forehead. The decisions were agonising and the responsibility placed on her shoulders was huge, but the triage system was well rehearsed and worked quickly and efficiently. Soldiers requiring surgery were moved to the two operating theatres and again assessed for priority. The intensive care unit, where nurse Kelli Mitchener worked, received patients as they came out of surgery. The medical team worked through the night. One patient was airlifted to Kandahar, where a higher level of care was available. His wounds were life threatening, but he and all the Australians survived—as did their much-loved Explosive Detection Dog Sarbi who turned up again 18 months after going missing during the gunfight.
A few days later, the patients who needed further treatment were airlifted out of Afghanistan, to the Middle East and then, in the RAAF’s first medical use of its new C-17 Globemaster aircraft, back to Australia. They were able to receive constant care from Wing Commander David Scott, one of the doctors who had treated them at Tarin Kowt, who had administered sophisticated pain relief for the flight home.
The medical care provided by Australians in Afghanistan was worlds apart from that in the Korean War. Wounded personnel were evacuated much faster. The average time taken to get a severely wounded patient to hospital fell from five hours in the Korean War (itself an improvement on ten hours in the Second World War) to just one hour in recent conflicts. The facilities that exist are better equipped and better organised. The wounded can be back in Australia for specialist care within days, not weeks. Survival rates have increased accordingly and there are many men and women who served in Iraq and Afghanistan who are alive today who would have died as a result of their wounds in previous conflicts.
Many features of the way medical care is organised have changed as well. In the 1950s, it would have been unthinkable for a woman to serve as a doctor in a combat zone, or for a man to be a nurse. Today 40 percent of the ADF’s nurses are male. Women serve in all medical roles including the most senior ADF medical officer, Commander Joint Health Air Vice-Marshal Tracy Smart AM.
Many of those who serve on deployments are reservists. Group Captain Holian is an RAAF reservist who works as an orthopaedic and trauma surgeon in civilian hospitals in Melbourne and Darwin when she is not on deployment with the RAAF to conflict zones and humanitarian disaster relief operations.
There is a constant interplay between civilian and military medicine. Wars have always stimulated medical research giving a renewed urgency to finding new treatments and techniques. In the First World War new surgical techniques and antiseptics were introduced; the Second World War saw the introduction of antibiotics and progress against malaria. And in recent years, the proportion of plasma given in blood transfusions to trauma patients has increased: a direct result of the experience of doctors in the war in Afghanistan, who found significant improvements in outcomes for patients who were given more plasma.
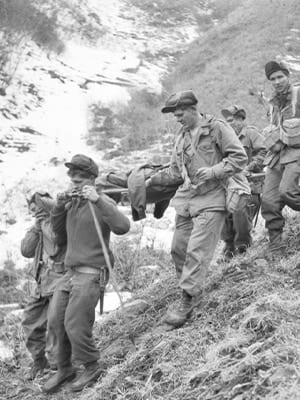
The changes in medical care for Australians in war and peacekeeping are the result of a long evolutionary process. The Korean War introduced advances such as the first limited use of helicopters for evacuation. During the Malayan Emergency (1948–60), Australian doctors developed an understanding of jungle warfare. During the Vietnam War (1962–75), helicopters came into their own as the main method of medical evacuation. Because evacuation was faster, men were surviving with injuries that would previously have killed them before they reached hospital. This required development of better systems of triage and trauma care. The clear advantages of these new systems in turn influenced civilian medicine, leading to the establishment of emergency medicine as a specialism in its own right in the United States and in Australia.
New drugs and technologies have played their part in the improvement of medical outcomes. For example, the new antimalarial drugs that were first tried in Vietnam. So too have improvements in the way care is organised and in a more rigorous approach to evaluating treatments.
A particular focus of recent efforts to improve military medical care has been in mental health treatment. During the Korean War and Vietnam War, mental health problems were often seen as short-term issues caused by ‘combat fatigue’ or poor morale. Treatment was focused on returning men to their units as quickly as possible.
Pressure for change first came outside the military from veterans of the Vietnam War. In the decades after the war, some veterans experienced serious long term mental health problems as a result of their service. The Vietnam Veterans Association of Australia pushed for an independent government funded counselling service. The Vietnam Veterans Counselling Service (VVCS, now the Veterans’ and Veterans’ Families Counselling Service) started operations in 1982. Initially focused on the needs of Vietnam veterans, its role has expanded to cover veterans of all conflicts and peacekeeping and their family members.
Within the Australian Defence Force, mental health screening is now given to all personnel returning from operations and help is available to those who need it. But there is still stigma attached to mental illness and many who would benefit from treatment do not seek it, for fear that being labelled with a mental health condition will limit or even end their career.
What has not changed in the years since 1945 are the personal qualities needed by those who work to heal the wounded and the sick. Consider Captain Carol Vaughan-Evans, an Australian Army doctor who was sent to the Kibeho refugee camp in Rwanda in 1995. As her team arrived at the camp, hostile forces of the Rwandan People’s Army (RPA) were attempting to intimidate its inhabitants into leaving. At the same time, members of the opposing interahamwe militia, themselves complicit in the previous genocide, sought to intimidate them to stay, attacking camp members with machetes. Captain Vaughan-Evans and her team treated the wounded. Over the next few days the situation deteriorated. On 22 April 1995, the RPA started firing into a crowd of refugees. Some 4,000 were killed. The Australians, outnumbered and forbidden by their rules of engagement from intervening, were powerless to stop the massacre and could only treat the wounded and count the dead. Despite the danger of gunfire, the medical team kept working.
At one point the RPA commander told Vaughan-Evans to leave the wounded patients, because the RPA were going to go in to ‘finish the rest off.’ She refused, showing great courage in returning to collect more wounded patients. For her actions she was awarded the Medal for Gallantry.
Captain Vaughan-Evans that day demonstrated the values that Australian doctors, nurses and other medical professionals have shown in service in war and peacekeeping since 1945: professionalism, born of long training; dedication, to keep going when the task seems unending; compassion, in the face of almost unimaginable suffering and trauma; and above all, humanity.
Author:
Dr Ian Jackson was Assistant Curator at the Shrine of Remembrance. Ian led the development of the Post ’45 section of the Galleries and curated the redevelopment of the Recent Conflicts gallery and the special exhibition For Humanity: Medicine in war and peacekeeping since 1945.
Updated